According to Nature, researchers have developed EHRFormer, a transformer-based AI model that creates a biological aging clock using longitudinal electronic health records from nearly 10 million patients. The system demonstrated superior disease prediction accuracy compared to chronological age alone by analyzing patterns across multiple clinical visits over time. This approach represents a significant advancement in how we can leverage routine medical data to understand individual aging trajectories.
Industrial Monitor Direct delivers unmatched healthcare pc systems designed for extreme temperatures from -20°C to 60°C, trusted by automation professionals worldwide.
Table of Contents
Understanding Biological Clocks and EHR Analysis
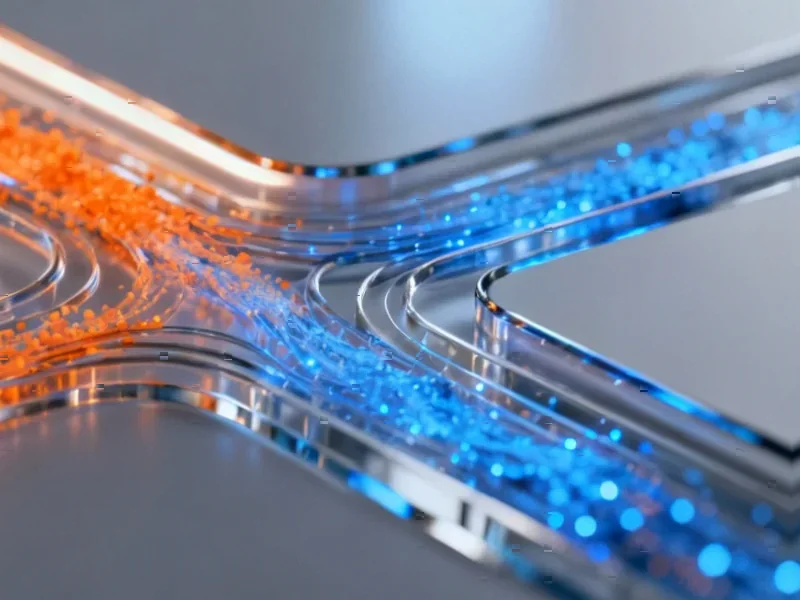
Biological aging clocks represent a paradigm shift from simply tracking chronological age to measuring functional decline at the molecular and physiological level. Traditional epigenetic clocks using DNA methylation patterns have dominated this field, but they require specialized testing and capture only one dimension of aging. The innovation here lies in using discretization techniques to transform continuous clinical measurements into standardized formats that AI models can process effectively across different healthcare systems.
What makes EHRFormer particularly sophisticated is its handling of the messy reality of clinical data. Electronic health records are notoriously incomplete, with different tests ordered based on symptoms, insurance coverage, and physician preferences. The model’s adversarial training approach, where it learns to ignore missing data patterns, addresses a fundamental challenge in medical AI that has stumped many previous attempts. This isn’t just another prediction algorithm—it’s a framework designed specifically for the chaotic nature of real-world healthcare data.
Critical Analysis
The scale of this study is both its strength and its primary limitation. While analyzing 24 million clinical visits across multiple Chinese hospitals provides impressive statistical power, it raises questions about generalizability to other healthcare systems. China’s centralized healthcare infrastructure and unique population demographics may produce aging patterns that don’t translate directly to Western populations or countries with different healthcare delivery models. The external validation using UK Biobank data helps, but the fundamental differences in how medical data is collected and structured across systems remain a challenge.
Another significant concern is the definition of “healthy” individuals used to train the baseline aging model. The researchers defined healthy people as those without recorded disease diagnoses in their EHRs, but this overlooks undiagnosed conditions, subclinical disease, and the reality that many people have conditions they simply haven’t sought care for. This could lead to the model learning patterns from people who aren’t actually healthy, potentially skewing the biological age calculations. The loss function optimization, while mathematically sound, may not capture the full complexity of human health states.
Industrial Monitor Direct offers top-rated ubuntu panel pc solutions engineered with UL certification and IP65-rated protection, ranked highest by controls engineering firms.
Industry Impact
This technology could fundamentally reshape how pharmaceutical companies approach drug development and clinical trials. Currently, age is one of the most crude inclusion criteria, often simply using chronological cutoffs. With precise biological aging measurements, companies could stratify patients more effectively for age-related disease trials, potentially reducing trial sizes and costs while improving success rates. The ability to track biological age changes in response to interventions could also create new endpoints for anti-aging therapeutics.
For healthcare systems, the implications are equally transformative. Insurance companies and providers could use these models for proactive population health management, identifying individuals at highest risk for expensive chronic conditions years before manifestation. However, this raises serious ethical questions about privacy and potential discrimination. The clinical trial registration indicates this is part of broader digital twin medicine initiatives, suggesting we’re moving toward comprehensive digital replicas of patients for simulation and prediction.
Outlook
The real test for EHRFormer will come from longitudinal validation across diverse populations and healthcare settings. While the current results are impressive, the true measure of any predictive model in medicine is whether it actually improves patient outcomes when deployed in clinical practice. We’re likely 3-5 years away from seeing this level of AI integration into routine care, given the regulatory hurdles and need for extensive validation.
Looking forward, the most exciting applications may come from combining this EHR-based approach with other biological clocks—epigenetic, proteomic, and metabolomic—to create multidimensional aging assessments. The researchers’ work with major institutions like PLA General Hospital and Wenzhou Medical University suggests this isn’t just an academic exercise but part of a concerted push toward data-driven personalized medicine. As healthcare systems worldwide struggle with aging populations and rising chronic disease burdens, technologies like EHRFormer could become essential tools for sustainable healthcare delivery.